Notes from the Northern Pacific Environmental Health Association Strategic Planning Meeting
These are my own rough and unofficial notes from the Northern Pacific Environmental Health Association Strategic Planning Meeting held on Pohnpei in May 2014.
There was a need identified to bring key actors together to develop a strategic plan. Environmental health touches on many areas – waste management, water, climate change, occupational safety. Consultants in health adaptation for climate change, specialists on vector borne diseases, specialists who advocate community based approaches.
Environmental health has a WHO definition. Includes human health, quality of life, that are determined by chemical, physical, biological, social and psychosocial factors in the environment. Assessing, correcting, controlling, and preventing those factors in the environment that can potential affect adversely the health of present and future generations.
Environmental health addresses all the physical, chemical, and biological factors external to a person, and all the related factors impacting behaviours. It encompasses the assessment and control of those environmental factors that can potentially affect health. It is targeted towards preventing disease and creating health-supportive environments. This definition excludes behaviour not related to environment, as well as behaviour related to the social and cultural environment, and genetics.
The definition was updated to specifically exclude some factors. The definition now excludes behavior not related to the environment, as well as behavior related to the social and cultural environment, and genetics. Target is preventing disease and creating health-supporting environments.
Environmental health services implement EH policies. Climate change health programming is a current focal area for EH.
Human rights and environmental health. Are clean and safe water, air, and food that are essential to our survival to be shared by all?
Or are they scarce economic resources like cars and computers that are optimized when they are subject to commercial pressures of supply and demand?
Human rights or market forces? Which should drive EH? Market forces tend to, however, have limited usefulness in EH. EH can work with markets, there are situations in which the economics are not there for commercial entities. EH should prioritize a human rights approach over an economic approach. Impoverished communities might be a low priority for safe drinking water, but EH must prioritize them based on human rights.
WHO estimates that one quarter of disease burden from EH risks. WHO recently reorganized from 30 areas to five areas of focus (2010 WHO report). EH is part of social, life cycle health efforts – promoting heath through life-course.
Worldwide 13 million deaths could be prevented annually by improving environmental health.
In children under 5 one third of all disease is environmentally linked.
Malaria, lower respiratory infection, and diarrhea are the three biggest killers of children around the world. All three can be impacted by improved environmental health.
85 of 102 categories of disease listed by WHO are influenced by EH factors.
Safe water, better hygiene, and cleaner fuels (indoor air pollution due to cooking in homes in the developing world is a major environmental health concern in some countries) are keys to better EH.
Safety of buildings, reduction of toxic substances in the home.
Northern Pacific EH challenges
Water, sanitation, and hygiene (WASH). Atoll countries have limited access to fresh water. Prone to drought and saline intrusion into potable water supplies through sea level rise. Atoll countries are the most vulnerable.
Dengue used to be under control, now there is a resurgence of dengue across the Pacific, most recently in Nauru. Climate factors may be involved.
Weather related health emergencies. Droughts in RMI. Floods in Solomon islands. Typhoons of record breaking strength. Disease accompanies/follows these events.
WHO is co-lead with UNICEF on health and nutrition. WASH cluster is under WHO.
Islands face waste management issues including health care waste. Asbestos risk profiles for north Pacific countries are incomplete. Occupational health and safety can be improved in most north Pacific countries.
FSM
Water, sanitation, and hygiene (WASH) remain a concern and focus especially given the history with cholera on Pohnpei and the number of diarrheal cases. Chuuk a particular concern due to overcrowded conditions, poor sanitation.
Typhoon. A risk for which preparation is possible.
Country redacted
One island has issues with secondary phosphate mining dust due to crushing and burning plant. Burned to remove water from phosphate. No worker protection. No dust control. Asthma among children in local neighborhood. No investigation: taboo. Main cash generator for government. In one family five children with severe asthma. Father set fire to conveyor belt. One month of damage. Eight year jail sentence. Pardoned after six years of jail. He did it to protest on behalf of his children. WHO was not invited to investigate. When a WHO representative did go he was told to stay away from the government owned phosphate mine. Elections have made some changes favorable to the people. The company is going to change old cooking machines. By December the company will be using new machines. Change is possible.
Goal is the development of a strategic plan for 2014-2017.
Palau has a national environmental health action plan, other nations should be developing theirs.
Components a strategic plan
Mission, vision, values, goals, strategies, action plans, programs for each goal, key performance indicators, monitoring and implementation of the plan.
Topics include food, water, air, vector-based disease (VDB), climate change (CCH), work (occupational).
WHO DPSEEA framework for EH. Driving forces, pressure, state, exposure, effects. Actions should impinge in the whole chain – the framework. You have to tackle the driving forces, the pressures, the state. The health sector will have to show leadership in challenging these sectors. Not just respond to effects.
Donor underneath this is ministry of environment of South Korea, Korea National Institute of Environmental research.
EH includes road safety.
CNMI. NPEHA. Began in Palau in 2003. Seven jurisdictions. Formation in 2003 focused on water sanitation. History of NPEHA. Early funding from Fiji school of medicine, AHEC, WHO.
WHO food safety sponsored NPEHA web site.
Funding is an ongoing challenge for EH officers. Currently funding is moving in climate change channels. Funding for EH is difficult to obtain, including a focus on climate change may increase the possible funding sources.
EH also faces a challenge of identity in some places. In nations where there are separate health and environment portfolios, EH can find itself in the empty space between the two. A recommendation was made that EH remain with health where possible. EH is more likely to draw WHO funding if under health than under environment.
EH has a stronger case to make as an agent of health than as an agent of environment. The focus on human illness and disease sees more funding from health sources than environmentally oriented sources. Hence the benefit of remaining under health.
RMI, Nauru, Palau, Kiribati, FSM will be last in country presentations later today.
Lunch break.
13:36 restart. Country profiles. RMI leads off. 29 atolls. 56000. 60% in Majuro and Kwajalein. 17.8 year median age. EH was formerly known as sanitation. Under MOH originally, then moved to EPA. Health promotion program remained in MOH. Food safety act completed in 2010. Food safety task force teams up health, EPA, R&D, education, and customs. Customs are important – front line receivers. First KRA to cross governmental units.
Food Safety and Quality control. Risk based food inspection deployed. 55 food establishments inspected in Majuro. Food packaging, labeling, temperature, quality control (expiration date), have authority to confiscate expired items.
Health promotion and disease prevention education. Community and school outreach. NCD coalition inaugurated in 2013. RMI is under an NCD emergency. Local gardening being promoted. In the outer islands. Not enough space in Majuro.
Water quality monitoring program. Officers are now certified (since 2008). Biannual certificatin by USEPA. 2013 participated in GEMS water quality test.
A national framework is being developed to assist communities at the household level manage and control waste.
Gaps. No national vector surveillance. Dengue hit RMI 2011 but no capacity in this area. Drought has also led to rise in diarrhea cases this year.
Strength: US EPA lab tech certification
Weakness: Capacity
Opportunity: Training and workshops are available
Vector-based disease awareness is being done in Samoa through the schools via science classes. Kids were trained to count mosquito larvae in containers and these were used as an early warning of mosquito population rise. Teachers gathered data. Integrated into science classes.
In the dengue outbreak in RMI, EPA asked government to reach out to Palau whose teams had the expertise to assist. Government turned instead to CDC. CDC team was a "South American" focused team. Flew in chems and controlled mosquitoes. Although assisted by EPA, there was no formal training of local capacity. At present there are boxes of supplies (and chemicals?) blocking access, in part, to the RMI EPA lab, other boxes elsewhere on the island. No central storage capacity, and insufficient training as to what to do with the supplies to avert future outbreaks. There is a tendency to turn to outside assistance which flies in, does the work, and they flies out with the skill sets needed to prevent future events. Region could be more interdependent, but external actors may not favor that, and local governments may not yet value the expertise sitting in a nearby neighbor.
Nauru. Population about 10,000. Now 12,000 with the boat people. Environmental health officers were originally known as "sanitarians." Currently one EHO expat and one health inspector with five assistants. Been in drought since 2011. RONADAPT: Republic of Nauru document on climate change.
Weaknesses in areas of legislation, lack of political will. No building codes. No occupational health safety regulations. Yet to be drafted. Gaps too in prosecution. Food safety is a weakness. Lack of dedicated officers. Food imports – lack of regulations. Prosecution is again a weakness. Vector-borne disease we have regular program, there is an ongoing dengue outbreak. There were 4 cases prior to last week, last week that rose to 15. Lack of source reduction. Public response needed. Australia brought in an etymologist working with EH to determine the species of mosquito. Issues involving quarantine and border control, they do not have the power to do anything at the border, there are food bans but foods still come in, lack of equipment, lack of trained staff due to turn-over, infrastructure issues, communication between units lacking, transparency.
Water sanitation checks are monthly on Nauru but focuses on government buildings. Needs expansion to businesses, hotels, restaurants, households. Limited test kits, limited lab capacity. Lab overwhelmed by medical issue testing, environmental is low priority in the lab. EH depends on med lab, no dedicated EH lab. There is only one health inspector.
Opportunities include WHO, NPEHA, PIHOA, FNU, SPC. Strengthening inter-sectoral commmunication. Legislation gaps could be closed.
Threats: political will or the lack thereof, sensitivity, public response. EH is always a sensitive issue. Public awareness is widespread.
At present there are three refugee camps. There will be five soon. The camps are in the interior of the island. They are crowded which leads to disease risk from a public health perspective. The camps may be linked to dengue outbreak, and may be sustaining the outbreak. Nauru has 14 districts. The majority of communities have accepted a proposal to have the Australian government build refugee housing in the districts. Women and children will be housed in the housing. The men will be retained in the camps while the women and children move into the communities. The women will be working – they are mostly Iranians and Iraqis with high level skill sets. The men, who were at the center of the rioting, represent a security issue and will be retained up at the camps. Remains to be seen how this will work out. The camps have treatment plants to treat sewage. Environmentally friendly as certified by outside agencies. The camps generate their own water. The boat people are not a burden to the local people. They generate their own power, they have their own health clinics, food is brought in for them.
There are no EPA regulations or laws per se, only public health regulations. There is no law protecting health. There is a need to pass laws to protect the health of the people. Water, air. Junked cars are probably contributing to dengue source. There is a need to revisit even the existing laws. Fines are still in shillings and pounds. There is a need to update existing laws, expand and adopt new laws and regulations to ensure the continued health and well being of the people.
Etymologist was brought in to Nauru by Aussie, in and out, to identify the mosquito. The dengue cases are scattered on the belt. Spray work has begun.
Palau.
Environmental health was basic sanitation, but as the nation grew, EH developed and expanded. While infectious diseases are well controlled and prevented, environmental health issues are more complex.
2004 developed National Environmental Health Action plan. Environmental health administration, community environmental health, consumer safety, vector control, emerging issues, cross-cutting, partnerships. Palau does environmental health inspection on a house to house basis. Waste management, water.
Palau reported to UN 100% of homes use a flush toilet. Solomons 53% lack toilet. Kiribati about 40%. Palau 0% lack toilet. The NEHAP was the advice of an NGO. Many countries ignored the NEHAP. Palau followed the NEHAP path. Palauans also have potable tap water. Palau is only country to approach WHO on air pollution and occupational health issues. Palau has great sensitivity in these areas. Air pollution is not an issue per se, but Palau is sensitive to these issues. Palau has been good at reaching out. When a shipment came in that was suspected to be asbestos, Palau sent samples to Korea and checked. Glass wool, not asbestos. But Palau really engaged in active good practices – customs checking with EH, getting the materials checked out.
Palau is on their second NEHAP which will carry them to 2015.
CNMI
Northernmost Micronesian island. Turn-over in leadership and staff an issue. 12 FTE staff covering three islands. BEH program has prioritized food safety. CNMI had a strong director. BEH is an opportunistic group and continues to participate in training.
No formal training program, just a lot of inter-departmental and intra-departmental training, taking advantage of what training is available as that training arises. Team in Saipan handles emergencies, ships, all hours of the day and night. BEH is semi-autonomous – dumped by government. Funding has declined 50% 2000-2013. The unit is apparently supposed to generate their own revenue.
Strengths: regulations are in place. Legislation exists to protect consumers. There are new grant opportunities under CDC ELC grant to territories.
There are issues of community political will to accept economic constraints. Prioritizing risk based assessment, shifting from descriptive assessment. Need to sustain and organize surveillance office. Information retention remains a challenge. We also need capacity building, no epidemiologist. A surveillance office that collects and maintains data is needed.
There is a need to increase education efforts, but limited personnel and funding are problematic.
New cultures are bringing new customs. Lunch delivery vehicles. Food sitting too long in a vehicle (take-out foods). There was another issue of food coming in contaminated with chemicals. A chemical had spilled or something like that.
New inspectors need ongoing training. Retention of experienced staff a problem. 20% of trained staff have left since 2010 for "greener pastures." The best trained and most capable are the ones that are lost.
Saipan is in bad shape financially. The austerity measures are undermining EH efforts. Retention is a broader issue. Funding cuts, unit cuts. Funding in Saipan is curative oriented, not preventative. EH remains at the mercy of hospital – hospital gets funding.
In Saipan the hospital is a separate entitity, some form of public corporation of five divisions, with four receiving some funding. Apparently EH was carved out and spun out under the hospital, something like that. Funding is problematic at best. Training is not funded. Sounds like EH has difficulty addressing areas that are not deemed important to the hospital corporation.
Kiribati.
Established in 1970s. EH responsible for food safety (60% of our time due to funding being there), water safety and security, sanitation, vector-control, climate change and DRM.
National Health Strategic Plan is not well aligned to EH concerns. Focus is on family planning, maternal and infant mortality.
1% of health budget goes to EH.
The higher rate of diarrhea in 2011 and 2012 are due to changes in data reporting and handling. Better data collection apparently.
Kiribati will begin GIS training for EH staff next month.
Weaknesses include a lack of a NEHAP, external funding required to reach outer islands. No government funding to do EH in outer islands. EH not a national health priority. Insufficient governmental support. No EH mandates in NHSP.
Public health ordinances date back to 1977. Quarantine also dates back to 1977. SPC has offered to provide funds to work on updating ordinances.
Tarawa faces challenges in terms of overcrowding – 9000 people per square kilometer. Maybe the highest in the world. Water a challenge. Two hours every second consecutive day. Many have private wells. Ground water pollution is a problem, contaminating the private wells. Hence the diarrhea issues and other water related health issues. "We are trying our best to stay alive." Saipan also has water rationing.
Kiribati participated in an Asian climate change and health conference, only Kiribati from the islands, which led to the development of a plan in coordination with the WHO. SPC picked up the WHO developed climate change health response plan for Kiribati and took it to the EU who agreed to fund the plan.
Climate change is a useful mechanism for obtaining core EH funding. No, we should not say that climate change is being included just to get funding, no, the reality is that climate change is driving health issues in Pacific island nations. Sea level rise impacts fresh water supplies impacts health. Kiribati is one of the least developed countries in the Pacific region which also makes them eligible for special UNDP funding. Kiribati also receiving MDG funding in some sectors.
FSM
Most states water quality is under state EPA except Kosrae where it remains under EH and department of health. EH role has diminished as state agencies and NGOs have risen. There is also a governmental downsizing. EH is always under the mercy of the hospital. Hospitals gets funded first and foremost, environmental health funding requests are fulfilled with available funds after hospitals are funded.
Partnerships are important here in the FSM due to the presence of states, NGOs and other agents.
FSM has no NEHAP/SEHAP. There is a chapter of the NCCHAP that includes vector, water, and food borne diseases, food security, malnutrition, landslides. National Climate Change Health Action Plan?
Food safety is an issue. Lack of food standards. Labeling. Street food – we are seeing a rapid increase in this area and we are probably behind in monitoring this area. Pounded food products – hard to track producers. Food handlers lack appropriate training. Diarrheal diseases.
Water quality and safety remain issues. Cases of diarrhea are high. Aging water systems are a problem too. Leaks need to be fixed to avoid contamination. EPA lacks water testing reagents. Cholera outbreaks have occurred. Cholera may follow drought.
There is also a lack of primary treatment for sewage in urban centers. Littering is problematic, backyard dump sites, waste management problem.
Vector-borne diseases have included dengue, zika, chikungunya. Filariasis still present, leptospirosis.
Strengths include work force and partners.
Weaknesses include lack of training opportunities
Opportunities include NPEHA SP/NCCHAP
Threats include lack of political will
WHO organization coming in June to FSM to work on updating national strategic health plans, environmental health should ensure they are represented at the table.
WHO, SPC, UNDP, are important partners for the countries in the presentations that were given today. These are the important partners and should be seen as such.
In some sense EH Is a victim of its own success and circumstances. At one time infectious diseases were the leading cause of death and EH was on the front line. Today NCD's are the leading cause of death, an area in which EH has little direct impact. The health funding is shifting towards dealing with the NCD emergency all Pacific island nations face. EH has to fight for scraps, gaining attention only when an environmentally sourced disease breaks out.
RMI: Water may be potable at the water plant source, but the aging distribution systems such as exist in RMI mean that at the far end of the pipe the water is not fit for human consumption. EH is left advising people to depend on their own rain tanks or alternate water sources.
Millennium Development Goals includes sanitation and water goals. Safe drinking water. Difficult to define safe. MDG calls for improved water, not safe water, which seems vague. That is the loop hole of the MDG statistics. Water may be unsafe to drink but somehow improved (less pathogenic). Some countries are reporting 78% of water improved yet cholera rate remains high. Improved but not potable, not safe.
Chlorinated water is a critical component of safe drinking water. Penetration of chlorinated water remains low across the Pacific.
Tuesday morning 2014 05 20 0910
Climate change and health.
Decadal average temperatures have been rising since 1850. z-scores. Annual average temperatures are run against a 30 year baseline using z-scores. The chart is using a 1961 baseline. Temperature rise is not uniform planet wide. Regional differences will be important in dealing with climate change.
In Sweden there are temperatures that no longer occur on the cold end. There are temperatures on the high end that were not seen before. The whole temperature distribution, roughly normal, is shifted up in temperature. Is the forcing human induced? IPCC 2013 ran models backwards using natural forcings and anthropogenic forcings. Only the models with anthropogenic forcings matched observations. Natural forcings could potentially explain the forcings up to 1960, but beyond 1960 only anthropogenic sources could produce the temperature rise seen since then.
The focus is on temperature, but other data from glaciers and ice sheets support the temperature data. Covers 2.5 and 6 degree rise models. Very little uncertainty in 2 degree rise models into 2040. Models projecting maximal adaptation and no adaptation, looked then at risk. Risks are moderate now but high degree of risk for Pacific islands even with adaptation by 2100 in 4 degree model.
Not just mean temperature is rising. Maximum temperatures are rising as well. Frequency and intensity of extreme events is rising. This is a concern. Stronger storms, deeper droughts, more frequent floods, more frequent storms. The record high for a 20 year return at present will be on a single year return rate by 2100. That is, the highest temperatures seen over a twenty year span of time will be seen every single year by 2100. Diseases that thrive on heat will gain traction across the globe.
Rainfalls amounts increase as atmosphere holds more water.
Risks and impacts. IPCC chart on climate, socioeconomic processes, impacts, and change.
A four degree rise will see a strong rise in food and water borne diseases – for food spoilage will be an issue. Mental, occupational, extreme weather events also see a strong rise in risk by 2080 to 2100. The biggest rise of risk, however, is undernutrition. Impacts on global food production will put large populations at risk of nutritional deficiencies.
Even if greenhouse gas emissions ended today, climate change would continue through 2040. Mitigation is all that can be done against the effects which are inevitable through 2040. Beyond 2040 policy changes today could change the path, but there has been little progress on reduction of greenhouse gas emissions.
These changes in the climate are permanent – they will not reverse. Adaptation is important.
Studying disease interactions with temperature is a field in its infancy. Salmonella increases by 1.2% per degree. Other enteric pathogens also increase with temperature. Rates of diarrhea increase globally. Population at risk of malaria increases with temperature. Malaria will continue to expand its range. In some areas malaria will go down: west Africa. Increased heat and water loss, increased drought, will lead to dryer conditions and reduce malaria but increase malnutrition and the potential for famine. Dengue range expands too.
Crop stress increases, crop yields are projected to decrease. There are already reductions. Food crop losses, even with adaptation especially in the tropics. Some areas may see upticks in production, rice productivity may spread north in north America.
Warming seas will drive tuna migration out of the waters of Palau, FSM, PNG, Nauru, RMI. Tuna shifts southeast to Tokelau, Kiribati, Cook, French Polynesia projected to see greatest gains.
1997-1998 was last big El Nino. El Nino conditions are developing again in the western Pacific.
Public health programs tend to plan for static health challenges. Stationary, however, is death. Change is coming. Planning for change must occur.
Wicked problems are insoluble problems, problems that can be made better or worse, but not resolved. They are often complex problems and improving one aspect of the problem may make others worse, or generate other problems to arise that did not previously exist. Climate change presents a wicked problem to public health. Wicked problems stems from social services where incomplete and contradictory information lead to insoluble situations.
Global Environment Facility. Set up to serve seven different... two major funds that serve us out here. Least developed country fund and special climate change fund. To get money the projects have to be country driven and represent country plans. Need a national adaptation plan to get funds. Certain categories of information are required to fill out a GEF form. A template is up on the projection screen.
Three to five outcomes generate three to five outputs. The preliminary application locks in funding amounts for each outcome, be careful. No programming changes, no reallocation, no transfer of funds between outcomes, outputs.
The special climate change funds have to show co-financing. GEF is minority contributor, but co-financing can be in-kind. You need to be able to estimate what you are doing now.
Project justification includes an overview, description, baseline scenario, stakeholders, risk, coordination.
Multi-country projects will have to have over-arching coordinated outcomes, outputs. The initial GEF, if funded, then gets an up to 200K to write the full proposal. But be careful, there is still the lock-in on the original outcomes in the GEF proposal. Amounts cannot be changed, but the proposal can then flesh out how those outcomes will be met – within the previously specified amount.
Fiji is using climate change funding. Samoa has GEF funding, Kiribati has EU funding for adaption. Vanuatu and two other partners are in an LDC GEF consortium.
GEF is not for research. GEF is for adaptation. If you need research, then unless you can fold that in under adaptation, research is not possible. LDC funds are easier to obtain, special climate change funds are harder to obtain at present.
Low and middle income countries can only access the special climate change fund. Only least developed countries are eligible for LDC GEF funding. Apparently Kiribati is an LDC, unclear where each other unit is.
There are USAID, EU, grants as well. Small grants have faster turn-around. Big GEF grants can require up to six years, although a new CEO is on board at GEF.
Kiribati is realizing about 500K per year under their grant. Provided there is a strong and stable governmental structure, big grants are possible. Only Nauru might have some difficulty in this regard – showing governmental support. There are issues at present that complicate matters for Nauru.
11:02 WHO. Vector borne diseases in the Pacific Island Countries.
Vector control. Filarial worms, plasmodia (malaria), arboviruses (arthropod borne virus) are carried by mosquitoes. No mosquito borne disease is totally under control. VBD characterized as zoonotic (animal reservoir) and non-zoonotic. West Nile has a base in animal and is transmitted to humans, others are have human reservoirs.
VBD incidences and outbreaks worsening in the Pacific. Unplanned development, poor water storage, high population densities, poor housing construction contribute to VBD load in Pacific. Spread of VBD enabled by travel and trade. People carry the diseases but sometimes the vector gets transported in goods.
Dengue, chikungunya, and zika are on the rise in the Pacific. Lymphatic filariasis and malaria are going down in incidence. Polyarthritus and Japanese encephalitis remain rare.
SPC chart of outbreaks across the Pacific at present. Chart from 7 April 2014. From ReliefWeb.
Dengue is a virus with no cure, no vaccine, no medicine. Only supportive care. Four types. Dengue 1, 2, 3, 4. Vaccines are 60% or less effective and only against three of the dengue strains. Vaccine is also very expensive. Not a promising near term option. Dengue is one of the fastest spreading diseases. Dengue is problematic due to the existence of the extreme form of dengue – dengue hemorrhagic fever. Asymptomatic cases exist in a population – could be as high as 80% of the cases are asymptomatic. So disease moves easily. Dengue is also passed by mother mosquito into eggs and dengue thus can live to survive another day in the offspring of the mother.
1844 first Hawaii epidemic.
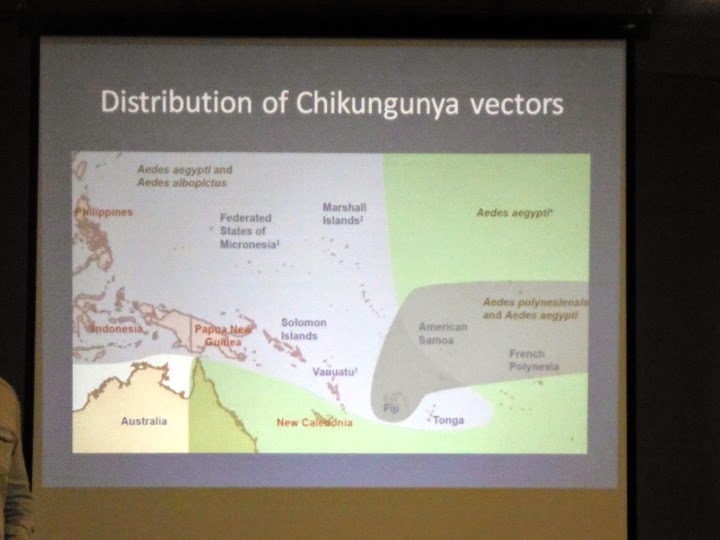
Chikungunya. Emerging disease. First seen in Tanzania in 1950s. Exported from Kenya to Reunion in 2005. Devastating outbreak. Over 250,000 people affected. 3-28% of cases are asymptomatic. The vector is Aedes aegypti and A. albopictus. This is the problem. The second vector can tolerate wide range of temperatures, humidities, and not a fussy eater, very adaptable. Can eat anything. Can breed in any container. Up to 18 months of excruciating joint pain but low mortality. High morbidity – long period of illness, but rarely resulting in death.
Aedes aegypti was original vector. But a mutation enhanced tranmission by Ae. albopictus. Both are prevalent in the Pacific. Also there are secondary potential vectors – scutellaris – Aedes polynesiensis.
Tonga currently in outbreak, 10,000 cases. Outbreaks can be explosive.
Zika. First seen in a monkey in 1947. Isolated in Nigeria 1968. Aedes aegypti in Malaysia tested positive in 1980s.
6000 cases in Micronesia in 2007. French Polynesia undergoing outbreak with over 30000 cases. Difficult to detect. No diagnostic tests. Lack of RDT and cross-reactivity a problem.
Lymphatic filariasis. Elephantitus. Culex mosquito is vector and Anopheles and Aedes in some cases. WHO has a program to eliminate this disease in the Pacific – only two drugs requires. Bendazole and one other. Aim is to eliminate in the Pacific by 2020.
Vector in Micronesia is Culex quinquefasciatus. Breeding in ponds. Brown house mosquito. Breeds anywhere there is high organic content water such as sewage water.
Micronesia has low epidemiology, has really pushed back on this disease.
Malaria has the largest global VBD footprint but not present in north Pacific. But the risk is there. Present in Solomons and Vanuatu. Vector is anopheles, a vector that is not present in the rest of the Pacific.
Refers to the Wallis line and notes that Solomons and Vanuatu are closer to southeast asia and Australia and share species with them.
Epidemic polyarthritis (Ross River virus). First isolated from Ross River, Queensland, 1959. Only 30% of population symptomatic. Range now includes PNG, Fiji, Cook, New Caledonia, Tonga, and Samoa. Zoonotic disease with reservoir in non-human hosts but human-mosquito-human transmission may occur. Main vectors are Aedes vigilax, Aedes polynesiensis, Culex annulirostrirs and Aedoes notoscriptus. The largest VBD in Australia, but less of an issue out in the Pacific.
Japanese encephalitis. Very important globally due to high mortality. But 98% of cases asymptomatic. But that 2% has a 40% mortality rate. 50000 cases annually, 15000 deaths. Reservoirs in pigs and birds.
Climate, vectors and diseases. Adult and immature mosquitoes require water for survival and development. Rate of development influenced by temperature. Seasonal activity of adults influenced by temperature. Incubation period of pathogens in mosquitoes also influenced by temperature. Ability of mosquito to survive until pathogen has incubated is dependent on favorable temperature and humidity.
Some pathogens take up to 12 days to incubate in the mosquito, but at a higher temperature the incubation period could drop to 8 days. Less chance of carrier dying before pathogen is transmissible. Mosquito production increases with temperature – more mosquitoes with higher temperatures.
Dengue induces strain specific immunity. So if you have an outbreak of type 3 in the Pacific, then that island will not likely see another type 3 outbreak for a decade or more – immunity exists in the population. And when three does reappear, it will affect only those who were either not infected in the earlier round or children born in the interim.
Initial testing of blood samples from Kosrae came back negative for dengue, zika, and chikungunya. A second set of samples has been sent out as the island has seen dengue like symptoms.
There was a need identified to bring key actors together to develop a strategic plan. Environmental health touches on many areas – waste management, water, climate change, occupational safety. Consultants in health adaptation for climate change, specialists on vector borne diseases, specialists who advocate community based approaches.
Environmental health has a WHO definition. Includes human health, quality of life, that are determined by chemical, physical, biological, social and psychosocial factors in the environment. Assessing, correcting, controlling, and preventing those factors in the environment that can potential affect adversely the health of present and future generations.
Environmental health addresses all the physical, chemical, and biological factors external to a person, and all the related factors impacting behaviours. It encompasses the assessment and control of those environmental factors that can potentially affect health. It is targeted towards preventing disease and creating health-supportive environments. This definition excludes behaviour not related to environment, as well as behaviour related to the social and cultural environment, and genetics.
The definition was updated to specifically exclude some factors. The definition now excludes behavior not related to the environment, as well as behavior related to the social and cultural environment, and genetics. Target is preventing disease and creating health-supporting environments.
Environmental health services implement EH policies. Climate change health programming is a current focal area for EH.
Human rights and environmental health. Are clean and safe water, air, and food that are essential to our survival to be shared by all?
Or are they scarce economic resources like cars and computers that are optimized when they are subject to commercial pressures of supply and demand?
Human rights or market forces? Which should drive EH? Market forces tend to, however, have limited usefulness in EH. EH can work with markets, there are situations in which the economics are not there for commercial entities. EH should prioritize a human rights approach over an economic approach. Impoverished communities might be a low priority for safe drinking water, but EH must prioritize them based on human rights.
WHO estimates that one quarter of disease burden from EH risks. WHO recently reorganized from 30 areas to five areas of focus (2010 WHO report). EH is part of social, life cycle health efforts – promoting heath through life-course.
Worldwide 13 million deaths could be prevented annually by improving environmental health.
In children under 5 one third of all disease is environmentally linked.
Malaria, lower respiratory infection, and diarrhea are the three biggest killers of children around the world. All three can be impacted by improved environmental health.
85 of 102 categories of disease listed by WHO are influenced by EH factors.
Safe water, better hygiene, and cleaner fuels (indoor air pollution due to cooking in homes in the developing world is a major environmental health concern in some countries) are keys to better EH.
Safety of buildings, reduction of toxic substances in the home.
Northern Pacific EH challenges
Water, sanitation, and hygiene (WASH). Atoll countries have limited access to fresh water. Prone to drought and saline intrusion into potable water supplies through sea level rise. Atoll countries are the most vulnerable.
Dengue used to be under control, now there is a resurgence of dengue across the Pacific, most recently in Nauru. Climate factors may be involved.
Weather related health emergencies. Droughts in RMI. Floods in Solomon islands. Typhoons of record breaking strength. Disease accompanies/follows these events.
WHO is co-lead with UNICEF on health and nutrition. WASH cluster is under WHO.
Islands face waste management issues including health care waste. Asbestos risk profiles for north Pacific countries are incomplete. Occupational health and safety can be improved in most north Pacific countries.
FSM
Water, sanitation, and hygiene (WASH) remain a concern and focus especially given the history with cholera on Pohnpei and the number of diarrheal cases. Chuuk a particular concern due to overcrowded conditions, poor sanitation.
Typhoon. A risk for which preparation is possible.
Country redacted
One island has issues with secondary phosphate mining dust due to crushing and burning plant. Burned to remove water from phosphate. No worker protection. No dust control. Asthma among children in local neighborhood. No investigation: taboo. Main cash generator for government. In one family five children with severe asthma. Father set fire to conveyor belt. One month of damage. Eight year jail sentence. Pardoned after six years of jail. He did it to protest on behalf of his children. WHO was not invited to investigate. When a WHO representative did go he was told to stay away from the government owned phosphate mine. Elections have made some changes favorable to the people. The company is going to change old cooking machines. By December the company will be using new machines. Change is possible.
Goal is the development of a strategic plan for 2014-2017.
Palau has a national environmental health action plan, other nations should be developing theirs.
Components a strategic plan
Mission, vision, values, goals, strategies, action plans, programs for each goal, key performance indicators, monitoring and implementation of the plan.
Topics include food, water, air, vector-based disease (VDB), climate change (CCH), work (occupational).
WHO DPSEEA framework for EH. Driving forces, pressure, state, exposure, effects. Actions should impinge in the whole chain – the framework. You have to tackle the driving forces, the pressures, the state. The health sector will have to show leadership in challenging these sectors. Not just respond to effects.
Donor underneath this is ministry of environment of South Korea, Korea National Institute of Environmental research.
EH includes road safety.
CNMI. NPEHA. Began in Palau in 2003. Seven jurisdictions. Formation in 2003 focused on water sanitation. History of NPEHA. Early funding from Fiji school of medicine, AHEC, WHO.
WHO food safety sponsored NPEHA web site.
Funding is an ongoing challenge for EH officers. Currently funding is moving in climate change channels. Funding for EH is difficult to obtain, including a focus on climate change may increase the possible funding sources.
EH also faces a challenge of identity in some places. In nations where there are separate health and environment portfolios, EH can find itself in the empty space between the two. A recommendation was made that EH remain with health where possible. EH is more likely to draw WHO funding if under health than under environment.
EH has a stronger case to make as an agent of health than as an agent of environment. The focus on human illness and disease sees more funding from health sources than environmentally oriented sources. Hence the benefit of remaining under health.
RMI, Nauru, Palau, Kiribati, FSM will be last in country presentations later today.
Lunch break.
13:36 restart. Country profiles. RMI leads off. 29 atolls. 56000. 60% in Majuro and Kwajalein. 17.8 year median age. EH was formerly known as sanitation. Under MOH originally, then moved to EPA. Health promotion program remained in MOH. Food safety act completed in 2010. Food safety task force teams up health, EPA, R&D, education, and customs. Customs are important – front line receivers. First KRA to cross governmental units.
Food Safety and Quality control. Risk based food inspection deployed. 55 food establishments inspected in Majuro. Food packaging, labeling, temperature, quality control (expiration date), have authority to confiscate expired items.
Health promotion and disease prevention education. Community and school outreach. NCD coalition inaugurated in 2013. RMI is under an NCD emergency. Local gardening being promoted. In the outer islands. Not enough space in Majuro.
Water quality monitoring program. Officers are now certified (since 2008). Biannual certificatin by USEPA. 2013 participated in GEMS water quality test.
A national framework is being developed to assist communities at the household level manage and control waste.
Gaps. No national vector surveillance. Dengue hit RMI 2011 but no capacity in this area. Drought has also led to rise in diarrhea cases this year.
Strength: US EPA lab tech certification
Weakness: Capacity
Opportunity: Training and workshops are available
Vector-based disease awareness is being done in Samoa through the schools via science classes. Kids were trained to count mosquito larvae in containers and these were used as an early warning of mosquito population rise. Teachers gathered data. Integrated into science classes.
In the dengue outbreak in RMI, EPA asked government to reach out to Palau whose teams had the expertise to assist. Government turned instead to CDC. CDC team was a "South American" focused team. Flew in chems and controlled mosquitoes. Although assisted by EPA, there was no formal training of local capacity. At present there are boxes of supplies (and chemicals?) blocking access, in part, to the RMI EPA lab, other boxes elsewhere on the island. No central storage capacity, and insufficient training as to what to do with the supplies to avert future outbreaks. There is a tendency to turn to outside assistance which flies in, does the work, and they flies out with the skill sets needed to prevent future events. Region could be more interdependent, but external actors may not favor that, and local governments may not yet value the expertise sitting in a nearby neighbor.
Nauru. Population about 10,000. Now 12,000 with the boat people. Environmental health officers were originally known as "sanitarians." Currently one EHO expat and one health inspector with five assistants. Been in drought since 2011. RONADAPT: Republic of Nauru document on climate change.
Weaknesses in areas of legislation, lack of political will. No building codes. No occupational health safety regulations. Yet to be drafted. Gaps too in prosecution. Food safety is a weakness. Lack of dedicated officers. Food imports – lack of regulations. Prosecution is again a weakness. Vector-borne disease we have regular program, there is an ongoing dengue outbreak. There were 4 cases prior to last week, last week that rose to 15. Lack of source reduction. Public response needed. Australia brought in an etymologist working with EH to determine the species of mosquito. Issues involving quarantine and border control, they do not have the power to do anything at the border, there are food bans but foods still come in, lack of equipment, lack of trained staff due to turn-over, infrastructure issues, communication between units lacking, transparency.
Water sanitation checks are monthly on Nauru but focuses on government buildings. Needs expansion to businesses, hotels, restaurants, households. Limited test kits, limited lab capacity. Lab overwhelmed by medical issue testing, environmental is low priority in the lab. EH depends on med lab, no dedicated EH lab. There is only one health inspector.
Opportunities include WHO, NPEHA, PIHOA, FNU, SPC. Strengthening inter-sectoral commmunication. Legislation gaps could be closed.
Threats: political will or the lack thereof, sensitivity, public response. EH is always a sensitive issue. Public awareness is widespread.
At present there are three refugee camps. There will be five soon. The camps are in the interior of the island. They are crowded which leads to disease risk from a public health perspective. The camps may be linked to dengue outbreak, and may be sustaining the outbreak. Nauru has 14 districts. The majority of communities have accepted a proposal to have the Australian government build refugee housing in the districts. Women and children will be housed in the housing. The men will be retained in the camps while the women and children move into the communities. The women will be working – they are mostly Iranians and Iraqis with high level skill sets. The men, who were at the center of the rioting, represent a security issue and will be retained up at the camps. Remains to be seen how this will work out. The camps have treatment plants to treat sewage. Environmentally friendly as certified by outside agencies. The camps generate their own water. The boat people are not a burden to the local people. They generate their own power, they have their own health clinics, food is brought in for them.
There are no EPA regulations or laws per se, only public health regulations. There is no law protecting health. There is a need to pass laws to protect the health of the people. Water, air. Junked cars are probably contributing to dengue source. There is a need to revisit even the existing laws. Fines are still in shillings and pounds. There is a need to update existing laws, expand and adopt new laws and regulations to ensure the continued health and well being of the people.
Etymologist was brought in to Nauru by Aussie, in and out, to identify the mosquito. The dengue cases are scattered on the belt. Spray work has begun.
Palau.
Environmental health was basic sanitation, but as the nation grew, EH developed and expanded. While infectious diseases are well controlled and prevented, environmental health issues are more complex.
2004 developed National Environmental Health Action plan. Environmental health administration, community environmental health, consumer safety, vector control, emerging issues, cross-cutting, partnerships. Palau does environmental health inspection on a house to house basis. Waste management, water.
Palau reported to UN 100% of homes use a flush toilet. Solomons 53% lack toilet. Kiribati about 40%. Palau 0% lack toilet. The NEHAP was the advice of an NGO. Many countries ignored the NEHAP. Palau followed the NEHAP path. Palauans also have potable tap water. Palau is only country to approach WHO on air pollution and occupational health issues. Palau has great sensitivity in these areas. Air pollution is not an issue per se, but Palau is sensitive to these issues. Palau has been good at reaching out. When a shipment came in that was suspected to be asbestos, Palau sent samples to Korea and checked. Glass wool, not asbestos. But Palau really engaged in active good practices – customs checking with EH, getting the materials checked out.
Palau is on their second NEHAP which will carry them to 2015.
CNMI
Northernmost Micronesian island. Turn-over in leadership and staff an issue. 12 FTE staff covering three islands. BEH program has prioritized food safety. CNMI had a strong director. BEH is an opportunistic group and continues to participate in training.
 |
Strengths: regulations are in place. Legislation exists to protect consumers. There are new grant opportunities under CDC ELC grant to territories.
There are issues of community political will to accept economic constraints. Prioritizing risk based assessment, shifting from descriptive assessment. Need to sustain and organize surveillance office. Information retention remains a challenge. We also need capacity building, no epidemiologist. A surveillance office that collects and maintains data is needed.
There is a need to increase education efforts, but limited personnel and funding are problematic.
New cultures are bringing new customs. Lunch delivery vehicles. Food sitting too long in a vehicle (take-out foods). There was another issue of food coming in contaminated with chemicals. A chemical had spilled or something like that.
New inspectors need ongoing training. Retention of experienced staff a problem. 20% of trained staff have left since 2010 for "greener pastures." The best trained and most capable are the ones that are lost.
Saipan is in bad shape financially. The austerity measures are undermining EH efforts. Retention is a broader issue. Funding cuts, unit cuts. Funding in Saipan is curative oriented, not preventative. EH remains at the mercy of hospital – hospital gets funding.
In Saipan the hospital is a separate entitity, some form of public corporation of five divisions, with four receiving some funding. Apparently EH was carved out and spun out under the hospital, something like that. Funding is problematic at best. Training is not funded. Sounds like EH has difficulty addressing areas that are not deemed important to the hospital corporation.
Kiribati.
Established in 1970s. EH responsible for food safety (60% of our time due to funding being there), water safety and security, sanitation, vector-control, climate change and DRM.
National Health Strategic Plan is not well aligned to EH concerns. Focus is on family planning, maternal and infant mortality.
1% of health budget goes to EH.
The higher rate of diarrhea in 2011 and 2012 are due to changes in data reporting and handling. Better data collection apparently.
Kiribati will begin GIS training for EH staff next month.
Weaknesses include a lack of a NEHAP, external funding required to reach outer islands. No government funding to do EH in outer islands. EH not a national health priority. Insufficient governmental support. No EH mandates in NHSP.
Public health ordinances date back to 1977. Quarantine also dates back to 1977. SPC has offered to provide funds to work on updating ordinances.
Tarawa faces challenges in terms of overcrowding – 9000 people per square kilometer. Maybe the highest in the world. Water a challenge. Two hours every second consecutive day. Many have private wells. Ground water pollution is a problem, contaminating the private wells. Hence the diarrhea issues and other water related health issues. "We are trying our best to stay alive." Saipan also has water rationing.
Kiribati participated in an Asian climate change and health conference, only Kiribati from the islands, which led to the development of a plan in coordination with the WHO. SPC picked up the WHO developed climate change health response plan for Kiribati and took it to the EU who agreed to fund the plan.
Climate change is a useful mechanism for obtaining core EH funding. No, we should not say that climate change is being included just to get funding, no, the reality is that climate change is driving health issues in Pacific island nations. Sea level rise impacts fresh water supplies impacts health. Kiribati is one of the least developed countries in the Pacific region which also makes them eligible for special UNDP funding. Kiribati also receiving MDG funding in some sectors.
FSM
Most states water quality is under state EPA except Kosrae where it remains under EH and department of health. EH role has diminished as state agencies and NGOs have risen. There is also a governmental downsizing. EH is always under the mercy of the hospital. Hospitals gets funded first and foremost, environmental health funding requests are fulfilled with available funds after hospitals are funded.
Partnerships are important here in the FSM due to the presence of states, NGOs and other agents.
Food safety is an issue. Lack of food standards. Labeling. Street food – we are seeing a rapid increase in this area and we are probably behind in monitoring this area. Pounded food products – hard to track producers. Food handlers lack appropriate training. Diarrheal diseases.
Water quality and safety remain issues. Cases of diarrhea are high. Aging water systems are a problem too. Leaks need to be fixed to avoid contamination. EPA lacks water testing reagents. Cholera outbreaks have occurred. Cholera may follow drought.
There is also a lack of primary treatment for sewage in urban centers. Littering is problematic, backyard dump sites, waste management problem.
Vector-borne diseases have included dengue, zika, chikungunya. Filariasis still present, leptospirosis.
Strengths include work force and partners.
Weaknesses include lack of training opportunities
Opportunities include NPEHA SP/NCCHAP
Threats include lack of political will
WHO organization coming in June to FSM to work on updating national strategic health plans, environmental health should ensure they are represented at the table.
WHO, SPC, UNDP, are important partners for the countries in the presentations that were given today. These are the important partners and should be seen as such.
In some sense EH Is a victim of its own success and circumstances. At one time infectious diseases were the leading cause of death and EH was on the front line. Today NCD's are the leading cause of death, an area in which EH has little direct impact. The health funding is shifting towards dealing with the NCD emergency all Pacific island nations face. EH has to fight for scraps, gaining attention only when an environmentally sourced disease breaks out.
RMI: Water may be potable at the water plant source, but the aging distribution systems such as exist in RMI mean that at the far end of the pipe the water is not fit for human consumption. EH is left advising people to depend on their own rain tanks or alternate water sources.
Millennium Development Goals includes sanitation and water goals. Safe drinking water. Difficult to define safe. MDG calls for improved water, not safe water, which seems vague. That is the loop hole of the MDG statistics. Water may be unsafe to drink but somehow improved (less pathogenic). Some countries are reporting 78% of water improved yet cholera rate remains high. Improved but not potable, not safe.
Chlorinated water is a critical component of safe drinking water. Penetration of chlorinated water remains low across the Pacific.
Tuesday morning 2014 05 20 0910
Climate change and health.
Decadal average temperatures have been rising since 1850. z-scores. Annual average temperatures are run against a 30 year baseline using z-scores. The chart is using a 1961 baseline. Temperature rise is not uniform planet wide. Regional differences will be important in dealing with climate change.
In Sweden there are temperatures that no longer occur on the cold end. There are temperatures on the high end that were not seen before. The whole temperature distribution, roughly normal, is shifted up in temperature. Is the forcing human induced? IPCC 2013 ran models backwards using natural forcings and anthropogenic forcings. Only the models with anthropogenic forcings matched observations. Natural forcings could potentially explain the forcings up to 1960, but beyond 1960 only anthropogenic sources could produce the temperature rise seen since then.
The focus is on temperature, but other data from glaciers and ice sheets support the temperature data. Covers 2.5 and 6 degree rise models. Very little uncertainty in 2 degree rise models into 2040. Models projecting maximal adaptation and no adaptation, looked then at risk. Risks are moderate now but high degree of risk for Pacific islands even with adaptation by 2100 in 4 degree model.
Not just mean temperature is rising. Maximum temperatures are rising as well. Frequency and intensity of extreme events is rising. This is a concern. Stronger storms, deeper droughts, more frequent floods, more frequent storms. The record high for a 20 year return at present will be on a single year return rate by 2100. That is, the highest temperatures seen over a twenty year span of time will be seen every single year by 2100. Diseases that thrive on heat will gain traction across the globe.
Rainfalls amounts increase as atmosphere holds more water.
Risks and impacts. IPCC chart on climate, socioeconomic processes, impacts, and change.
A four degree rise will see a strong rise in food and water borne diseases – for food spoilage will be an issue. Mental, occupational, extreme weather events also see a strong rise in risk by 2080 to 2100. The biggest rise of risk, however, is undernutrition. Impacts on global food production will put large populations at risk of nutritional deficiencies.
Even if greenhouse gas emissions ended today, climate change would continue through 2040. Mitigation is all that can be done against the effects which are inevitable through 2040. Beyond 2040 policy changes today could change the path, but there has been little progress on reduction of greenhouse gas emissions.
These changes in the climate are permanent – they will not reverse. Adaptation is important.
Studying disease interactions with temperature is a field in its infancy. Salmonella increases by 1.2% per degree. Other enteric pathogens also increase with temperature. Rates of diarrhea increase globally. Population at risk of malaria increases with temperature. Malaria will continue to expand its range. In some areas malaria will go down: west Africa. Increased heat and water loss, increased drought, will lead to dryer conditions and reduce malaria but increase malnutrition and the potential for famine. Dengue range expands too.
Crop stress increases, crop yields are projected to decrease. There are already reductions. Food crop losses, even with adaptation especially in the tropics. Some areas may see upticks in production, rice productivity may spread north in north America.
Warming seas will drive tuna migration out of the waters of Palau, FSM, PNG, Nauru, RMI. Tuna shifts southeast to Tokelau, Kiribati, Cook, French Polynesia projected to see greatest gains.
1997-1998 was last big El Nino. El Nino conditions are developing again in the western Pacific.
Public health programs tend to plan for static health challenges. Stationary, however, is death. Change is coming. Planning for change must occur.
Wicked problems are insoluble problems, problems that can be made better or worse, but not resolved. They are often complex problems and improving one aspect of the problem may make others worse, or generate other problems to arise that did not previously exist. Climate change presents a wicked problem to public health. Wicked problems stems from social services where incomplete and contradictory information lead to insoluble situations.
Global Environment Facility. Set up to serve seven different... two major funds that serve us out here. Least developed country fund and special climate change fund. To get money the projects have to be country driven and represent country plans. Need a national adaptation plan to get funds. Certain categories of information are required to fill out a GEF form. A template is up on the projection screen.
Three to five outcomes generate three to five outputs. The preliminary application locks in funding amounts for each outcome, be careful. No programming changes, no reallocation, no transfer of funds between outcomes, outputs.
The special climate change funds have to show co-financing. GEF is minority contributor, but co-financing can be in-kind. You need to be able to estimate what you are doing now.
Project justification includes an overview, description, baseline scenario, stakeholders, risk, coordination.
Multi-country projects will have to have over-arching coordinated outcomes, outputs. The initial GEF, if funded, then gets an up to 200K to write the full proposal. But be careful, there is still the lock-in on the original outcomes in the GEF proposal. Amounts cannot be changed, but the proposal can then flesh out how those outcomes will be met – within the previously specified amount.
Fiji is using climate change funding. Samoa has GEF funding, Kiribati has EU funding for adaption. Vanuatu and two other partners are in an LDC GEF consortium.
GEF is not for research. GEF is for adaptation. If you need research, then unless you can fold that in under adaptation, research is not possible. LDC funds are easier to obtain, special climate change funds are harder to obtain at present.
Low and middle income countries can only access the special climate change fund. Only least developed countries are eligible for LDC GEF funding. Apparently Kiribati is an LDC, unclear where each other unit is.
There are USAID, EU, grants as well. Small grants have faster turn-around. Big GEF grants can require up to six years, although a new CEO is on board at GEF.
Kiribati is realizing about 500K per year under their grant. Provided there is a strong and stable governmental structure, big grants are possible. Only Nauru might have some difficulty in this regard – showing governmental support. There are issues at present that complicate matters for Nauru.
11:02 WHO. Vector borne diseases in the Pacific Island Countries.
Vector control. Filarial worms, plasmodia (malaria), arboviruses (arthropod borne virus) are carried by mosquitoes. No mosquito borne disease is totally under control. VBD characterized as zoonotic (animal reservoir) and non-zoonotic. West Nile has a base in animal and is transmitted to humans, others are have human reservoirs.
VBD incidences and outbreaks worsening in the Pacific. Unplanned development, poor water storage, high population densities, poor housing construction contribute to VBD load in Pacific. Spread of VBD enabled by travel and trade. People carry the diseases but sometimes the vector gets transported in goods.
Dengue, chikungunya, and zika are on the rise in the Pacific. Lymphatic filariasis and malaria are going down in incidence. Polyarthritus and Japanese encephalitis remain rare.
 |
| http://reliefweb.int/sites/reliefweb.int/files/resources/Map-D-C-Z.pdf |
SPC chart of outbreaks across the Pacific at present. Chart from 7 April 2014. From ReliefWeb.
Dengue is a virus with no cure, no vaccine, no medicine. Only supportive care. Four types. Dengue 1, 2, 3, 4. Vaccines are 60% or less effective and only against three of the dengue strains. Vaccine is also very expensive. Not a promising near term option. Dengue is one of the fastest spreading diseases. Dengue is problematic due to the existence of the extreme form of dengue – dengue hemorrhagic fever. Asymptomatic cases exist in a population – could be as high as 80% of the cases are asymptomatic. So disease moves easily. Dengue is also passed by mother mosquito into eggs and dengue thus can live to survive another day in the offspring of the mother.
1844 first Hawaii epidemic.
Chikungunya. Emerging disease. First seen in Tanzania in 1950s. Exported from Kenya to Reunion in 2005. Devastating outbreak. Over 250,000 people affected. 3-28% of cases are asymptomatic. The vector is Aedes aegypti and A. albopictus. This is the problem. The second vector can tolerate wide range of temperatures, humidities, and not a fussy eater, very adaptable. Can eat anything. Can breed in any container. Up to 18 months of excruciating joint pain but low mortality. High morbidity – long period of illness, but rarely resulting in death.
Aedes aegypti was original vector. But a mutation enhanced tranmission by Ae. albopictus. Both are prevalent in the Pacific. Also there are secondary potential vectors – scutellaris – Aedes polynesiensis.
Tonga currently in outbreak, 10,000 cases. Outbreaks can be explosive.
Zika. First seen in a monkey in 1947. Isolated in Nigeria 1968. Aedes aegypti in Malaysia tested positive in 1980s.
6000 cases in Micronesia in 2007. French Polynesia undergoing outbreak with over 30000 cases. Difficult to detect. No diagnostic tests. Lack of RDT and cross-reactivity a problem.
Lymphatic filariasis. Elephantitus. Culex mosquito is vector and Anopheles and Aedes in some cases. WHO has a program to eliminate this disease in the Pacific – only two drugs requires. Bendazole and one other. Aim is to eliminate in the Pacific by 2020.
Vector in Micronesia is Culex quinquefasciatus. Breeding in ponds. Brown house mosquito. Breeds anywhere there is high organic content water such as sewage water.
Micronesia has low epidemiology, has really pushed back on this disease.
Malaria has the largest global VBD footprint but not present in north Pacific. But the risk is there. Present in Solomons and Vanuatu. Vector is anopheles, a vector that is not present in the rest of the Pacific.
Refers to the Wallis line and notes that Solomons and Vanuatu are closer to southeast asia and Australia and share species with them.
Epidemic polyarthritis (Ross River virus). First isolated from Ross River, Queensland, 1959. Only 30% of population symptomatic. Range now includes PNG, Fiji, Cook, New Caledonia, Tonga, and Samoa. Zoonotic disease with reservoir in non-human hosts but human-mosquito-human transmission may occur. Main vectors are Aedes vigilax, Aedes polynesiensis, Culex annulirostrirs and Aedoes notoscriptus. The largest VBD in Australia, but less of an issue out in the Pacific.
Japanese encephalitis. Very important globally due to high mortality. But 98% of cases asymptomatic. But that 2% has a 40% mortality rate. 50000 cases annually, 15000 deaths. Reservoirs in pigs and birds.
Climate, vectors and diseases. Adult and immature mosquitoes require water for survival and development. Rate of development influenced by temperature. Seasonal activity of adults influenced by temperature. Incubation period of pathogens in mosquitoes also influenced by temperature. Ability of mosquito to survive until pathogen has incubated is dependent on favorable temperature and humidity.
Some pathogens take up to 12 days to incubate in the mosquito, but at a higher temperature the incubation period could drop to 8 days. Less chance of carrier dying before pathogen is transmissible. Mosquito production increases with temperature – more mosquitoes with higher temperatures.
Dengue induces strain specific immunity. So if you have an outbreak of type 3 in the Pacific, then that island will not likely see another type 3 outbreak for a decade or more – immunity exists in the population. And when three does reappear, it will affect only those who were either not infected in the earlier round or children born in the interim.
Initial testing of blood samples from Kosrae came back negative for dengue, zika, and chikungunya. A second set of samples has been sent out as the island has seen dengue like symptoms.





















Comments
Post a Comment